"Purchase glyset 50mg visa, ".
By: M. Dargoth, M.A., M.D., Ph.D.
Co-Director, Dell Medical School at The University of Texas at Austin
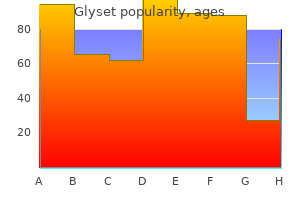
Finally cheap 50 mg glyset visa, an exercise prescription should be written on a prescription pad to strengthen the endorsement for increased physical activity order 50mg glyset with mastercard. It is important to "start low and go slow discount glyset amex," especially if the older adult has been relatively sedentary buy generic glyset 50 mg. It is more important to get the older adult to do any physical activity than to prescribe something that is unattainable. The health of older adults may be better served if they perform a little more exercise or activity than the previous week, attempting to incorporate the activity into their normal daily lives such as walking to a store or gardening. The goal should be for the person to feel "pleasantly" tired a few hours after the activity with the aim of increasing the activity slowly until a desired level of fitness is obtained. Promotion of an active lifestyle is important at all ages and the benefits to older adults are numerous. Health care providers need to realize that for exercise to be beneficial it need not be strenuous or prolonged. Just encouraging patients to get up out of their chairs and start moving will improve not only the quality, but the quantity, of disabilityfree years. A priority in screening should be given to preventive services that are both easy to deliver and associated with beneficial outcomes. Physical Activity in Older Adults Exercise and physical activity as a form of primary prevention have many benefits even for sedentary older adults. A recent meta-analysis of physical activity and well-being in advanced age concluded that physical activity had its strongest effect on self-efficacy (self-confidence), and improvements in cardiovascular status, strength, and functional capacity also improved well-being. Lifestyle physical activities that are more unstructured as compared with a formal exercise plan are being shown to increase levels of physical activity in sedentary populations. DiPietro L: Physical activity in aging: changes in patterns and their relationship to health and function. As individuals age, chronic diseases, functional impairments, polypharmacy, and age-related physiologic and socioeconomic changes may all act in concert to place an older adult nutritionally at risk. Health care providers, however, rarely take the time to consider the diet and nutritional status of their patients. Poor nutritional status may be the result of too little dietary intake leading to malnutrition, too much dietary content for actual expenditure leading to obesity, and inappropriate dietary intake exacerbating such conditions as diabetes, hypertension, and renal insufficiency. Obesity tends to be a problem for patients younger than 75 years, whereas undernutrition is commonly encountered in those older than 85. Although animal studies have indicated increased longevity with lower body weight and caloric restriction without malnutrition, studies on the relative risk of obesity to mortality in older adults are inconsistent, ranging from a protective effect for hip fractures to increased functional disability. A multitude of interrelated factors can place an older adult at nutritional risk (Table 39-9 and Table 39-10). Because anorexia, weight loss, and undernutrition in older persons have such deleterious effects, factors that can be treated or reversed are of major importance. Treatment with orexigenic agents to promote weight gain is controversial but should be considered. Megestrol acetate in doses up to 800 mg per day increases weight (fat mass) in older persons and must be used with caution if the individual has a history of clotting disorders. Dronabinol, a cannabis derivative, can enhance weight gain but has a tendency to cause dysphoria in the elderly, which limits its usefulness. A dietician can assist the primary care physician in formulating a weight loss program for older patients, with a goal of 0. Promotion of a balanced, healthy diet for all older adults, including recognition and remediation of macronutrient deficiencies, should be incorporated into the health promotion strategies of all primary care physicians caring for older adults. Recommending weight loss, especially to an older individual should be done with caution because weight loss in general carries a poor prognosis. For patients younger than 70 years of age who are 20% above ideal body weight, prudent weight loss should be recommended. For patients older than 70, if a medical condition is likely to be significantly improved by prudent dieting then it should be recommended. Such conditions would include severe hypertension, back pain from obesity, degenerative joint disease, gait and balance problems, and diabetes mellitus.
Greenberg P et al: the economic burden of depression in the United States: how did it change between 1990 and 2000 Preventive interventions may include psychoeducation about the particular challenges being confronted order glyset with american express, stresscoping techniques purchase genuine glyset online, the use of problem-solving therapies to help patients cope more effectively with increasing limitations discount 50 mg glyset visa, supporting general health and wellness (good nutrition/ exercise/relaxation) purchase glyset with a mastercard, facilitating support of family/friends/ support groups, and protecting sleep quality through better sleep hygiene. Prevention strategies for addressing depression in the elderly have also been shown to be effective in the primary care setting. Over the past decade, it has become clear that antidepressant treatments can have a very favorable impact on the long-term course of depressive illness, particularly in preventing recurrences of disease. In addition, because symptoms and signs of depression are frequently masked by other medical conditions, health care providers treating individuals with chronic diseases may not recognize that the underlying cause of depressed mood, decreased energy, sleep changes, or appetite changes is depression. Therefore, a high index of suspicion of depression should be maintained when treating patients who present with symptoms and signs of chronic physical conditions, multiple somatic complaints, or chronic pain complaints. Screening should be utilized in these instances populations with consistent systems in place for diagnosis, treatment, and follow-up. The American Heart Association and the American Psychiatric Association specifically recommend screening for depression in patients with coronary heart disease. Depression and Other Chronic Illnesses Depression commonly co-occurs with chronic diseases, complicating treatment and worsening chronic disease outcome. Depression is an independent risk factor in the development of cardiovascular diseases (heart disease, stroke). Screening, diagnosis, and treatment of depression could have an impact on the course and management of chronic diseases Although approximately one-third of individuals with chronic medical conditions may experience symptoms of Table 52-2. Cancer Type Breast Colon Gynecological Lung Lymphomas Oropharyngeal Pancreatic Prevalence of Depression (%) 1. Impact of Health Disparities Overall, studies show that disparities exist between whites and racially and ethnically diverse groups in mental health status, in utilization of mental health services, in quality of care and outcome regardless of socioeconomic status in the four major underserved ethnic and racial groups: African Americans, American Indians, Asian Americans, and Hispanics. Risk of mental illness and poor mental health outcomes in diverse and underserved populations is increased due to nonfamilial factors associated with depression (eg, socioeconomic status, environmental factors, access to health care, and higher rates of health disorders). Despite increases in the rate of antidepressant medication use over the past 12 years among all racial and ethnic groups, this increase has been disproportionately higher in whites compared with non-Hispanic blacks. The increased risk of living in poverty with inadequate access to health care and inadequate treatment, more prevalent in populations of color, may multiply stress and contribute to persistent and recurring episodes of depression. For nonwhite populations, the chronic stress of discrimination and subsequent effects on immune regulation of living as a member of a marginalized racial and ethnic group can also contribute to depression. Because of the independent increased risk of chronic diseases and mental illness in diverse racial and ethnic populations, the impact of mental illness on chronic diseases is increased substantially. Applied Research Center and Northwest Federation of Community Organizations: Closing the Gap: Solutions to RaceBased Health Disparities, 2005. Only 20%-30% of patients with emotional or psychological issues report these to their primary care physicians, and the most common somatic symptom reported by more than half of patients with major depression was "feeling fatigued, weak, or tired all over. Initial assessment should include a focused psychiatric history and examination and, for older adults, a brief clinical cognitive examination. In addition, a medical history, physical examination, focused neurologic examination, and laboratory studies to rule out physical conditions with similar symptoms are preferred as part of the assessment. It is also important to assess other domains, particularly for older adults, including level of functioning or disability, loss or grief concerns, physical environment, and psychosocial situation. In more than 90% of patients diagnosed with a major depressive disorder (characterized by several major depressive episodes), two of these nine features are present: depressed mood or anhedonia (the loss of interest or pleasure) Clinical Findings the type and level of severity of depression runs along a spectrum, ranging from subclinical varieties to major depression. Major depression typically occurs in episodes, each with a clear beginning and end. After an initial episode, more than 50% will have additional episodes in their lifetime. Among older adults with depression, about half had experienced depression earlier in their life, the other half experience it for the first time after the age of 60. Initial Assessment the American Academy of Family Physicians states that mental health services are an integral component of the continuum of care in the primary care setting. However, the reluctance of individuals to seek care for mental health problems along with a likelihood of somatization of emotional issues pose giant obstacles for mental health care in these settings. A total of five of the nine features, including one of the first two, must be present during this same 2-week period for the patient to be diagnosed with the disorder.
Hypertension can also be related to excessive use of caffeine purchase glyset 50mg without prescription, ingestion of licorice purchase 50mg glyset otc, or use of illicit drugs such as cocaine or amphetamines buy glyset 50 mg with amex. Hypertension can also occur secondary to acute and chronic kidney disease buy generic glyset 50 mg, which might be suggested by a flank mass, elevated creatinine level, or abnormal findings such as proteinuria, hematuria, or casts on routine urinalysis. Rarely, hypertension may be related to renal artery stenosis, particularly if onset is before the age of 20 or after the age of 50 years. Other causes to consider in the differential diagnosis include hypo- or hyperthyroidism, primary hyperaldosteronism, Cushing syndrome, coarctation of the aorta, pheochromocytoma, and sleep apnea syndrome in the appropriate clinical presentation. Prevention A healthy lifestyle is hailed both as prevention and as initial therapy for hypertension (Table 34-3). Clinical Findings Before patients with hypertension can be offered adequate treatment, they must be properly diagnosed. Because patients are often asymptomatic, the risk factors for hypertension must be understood and appropriate patients screened. In addition to the modifiable risk factors noted earlier, there are nonmodifiable factors, including African-American race, family history of hypertension, and increasing age. Any prior history of hypertension should be elicited as well as response and side effects to any previous hypertension therapy. It is important to inquire about any history or symptoms suggestive of coronary artery disease or other significant comorbidities, including diabetes mellitus, heart failure, dyslipidemia, renal disease, and peripheral vascular disease. The family history should also be reviewed, with special attention to the presence of hypertension, premature coronary artery disease, diabetes, renal disease, dyslipidemia, or stroke. Use of tobacco, alcohol, or illicit drugs should be documented, as well as dietary intake of sodium, saturated fat, and caffeine. Current medications used by the patient should be reviewed, including over-the-counter medications and herbal formulations. Physical examination-The initial physical examination should be comprehensive and should pay careful attention to the areas outlined in Table 34-4. In some patients, the presence of hypertension may be signaled by early morning headaches or, in those with severe hypertension, by signs or symptoms associated with target organ damage. Such symptoms might include nausea, vomiting, visual disturbance, chest pain, or confusion. For proper measurement of blood pressure, the patient should be seated in a chair with his or her back supported and the arm bared and supported at heart level. Caffeine and tobacco should be avoided in the 30 minutes preceding measurement, and measurement should begin after 5 minutes of rest. It is important that the diagnosis be made after the elevation of blood pressure is documented with three separate readings, on three different occasions, unless the elevation is severe or is associated with symptoms requiring immediate attention (hypertensive urgency or emergency). In cases in which the diagnosis is in question, properly taken home blood pressure measurements can be useful. These classifications are based on the average of two or more provider-obtained blood pressure measurements from a seated patient. Self-monitoring-Patients should be encouraged to do self-monitoring of their blood pressure at home. Many easyto-use blood pressure monitors are commercially available at reasonable cost for use at home. Validated electronic devices are recommended, and independent reviews of available devices, such as that published by Consumer Reports, are available to assist the consumer. Self-measurement can be helpful, not only in establishing the diagnosis of hypertension, but also in assessing response to medical therapy, and in encouraging patient compliance with therapy by providing regular feedback on therapy response. Component of Examination General Assessment Focus Baseline height, weight, and waist circumference Upper and lower extremity blood pressure measurement to assess for coarctation of the aorta Features of Cushing syndrome Funduscopic examination for signs of hypertensive retinopathy (eg, arteriolar narrowing, focal arteriolar constriction, atrioventricular nicking, hemorrhages, exudates) Carotid bruits Neck vein distention or thyroid gland enlargement Abnormalities in rate, rhythm, murmurs, or extra heart sounds Rales, rhonchi, or wheezes Abdominal bruits suggestive of renal artery stenosis Enlargement of kidneys (mass) or aortic pulsation suggesting aneurysm Diminished or absent peripheral arterial pulsations Edema Signs of vascular compromise Neurologic deficits Eyes Neck Heart Lungs Abdomen B. Urinalysis should be assessed for evidence of hematuria, proteinuria, or casts suggestive of intrinsic renal disease. Potassium levels help assess for hyper-aldosteronism, and creatinine levels reflect renal function. The fasting blood glucose level is used to assess for diabetes mellitus, and the lipid profile is an indicator of cardiovascular risk. Additional tests to consider include hemoglobin A1c, thyroid-stimulating hormone, urine microalbumin, creatinine clearance, and 24-hour urine for protein.